Surgical Approaches to Rhinoplasty
The field of rhinoplasty encompasses various surgical techniques, each designed to address specific anatomical concerns while minimizing visible scarring and recovery time. Understanding these different approaches helps patients make informed decisions about their treatment and set appropriate expectations for their surgical experience.
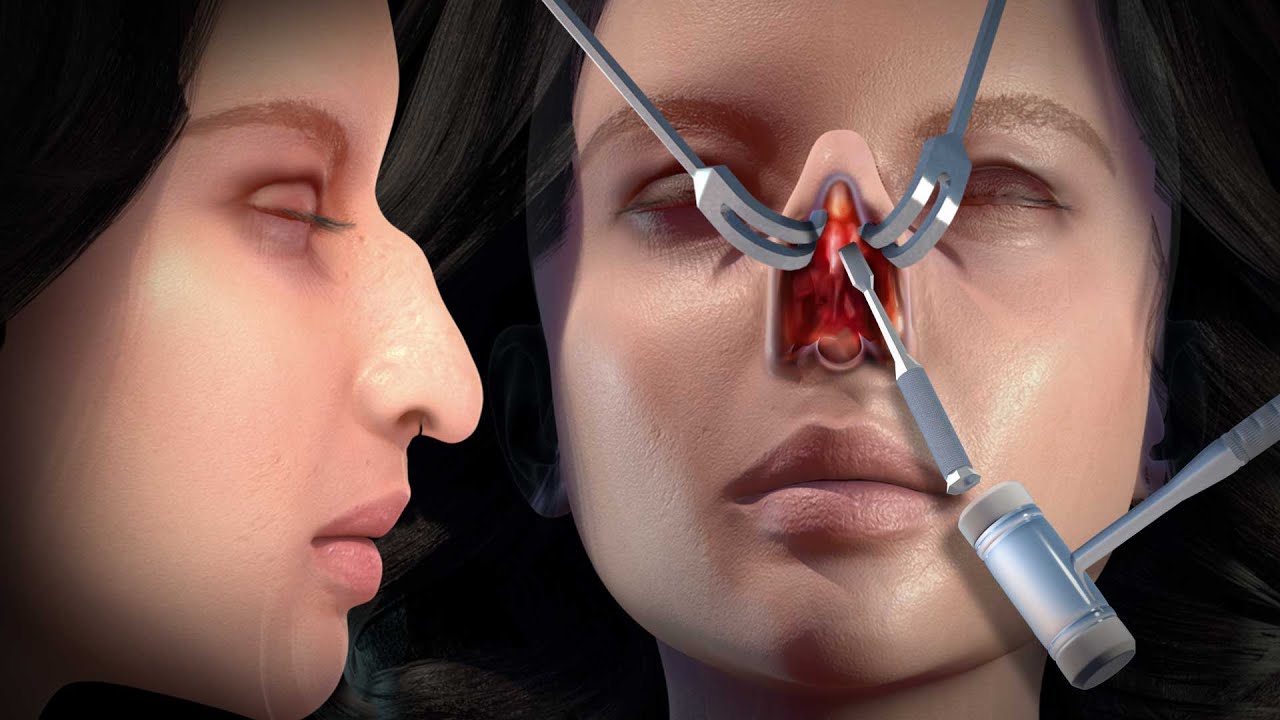
Open Rhinoplasty
Open rhinoplasty, also known as external rhinoplasty, involves creating a small incision across the columella—the strip of tissue separating the nostrils. This approach provides the surgeon with direct visualization of the nasal structures, making it the preferred technique for complex cases requiring extensive reshaping or reconstruction.
The open approach offers several significant advantages. The enhanced visibility allows surgeons to precisely assess and modify nasal anatomy, making it ideal for cases involving significant tip work, asymmetry correction, or revision surgery. Surgeons can directly see how modifications affect the overall nasal structure, leading to more predictable outcomes. The technique also facilitates teaching and documentation, as the surgical field is clearly visible.
The primary concern patients have about open rhinoplasty is the external scar across the columella. However, when performed by an experienced surgeon, this incision typically heals to become virtually imperceptible. The scar is placed in the natural crease of the columella and usually fades significantly within several months. Most patients find that the benefits of improved surgical precision far outweigh concerns about minimal scarring.
Best suited for: Complex tip work, revision rhinoplasty, significant asymmetry correction, ethnic rhinoplasty requiring major structural changes, and cases requiring cartilage grafting.
Closed Rhinoplasty
Closed rhinoplasty, or endonasal rhinoplasty, involves making all incisions inside the nostrils, leaving no external scars. This traditional approach has been refined over decades and remains an excellent option for appropriate candidates. The technique requires exceptional surgical skill, as the surgeon must work through limited access points without direct visualization of all nasal structures.
The closed approach offers several benefits, including no external scarring, potentially less swelling in the immediate post-operative period, and slightly shorter operative time. The preservation of the columellar skin and its blood supply may contribute to faster initial healing. Many surgeons who specialize in closed rhinoplasty develop extraordinary tactile skills and spatial awareness that allow them to achieve excellent results through this approach.
However, closed rhinoplasty has limitations. The restricted visualization makes it less suitable for complex cases, particularly those involving significant tip work or revision surgery. The technique requires extensive surgical experience and is generally reserved for less complicated procedures such as dorsal hump reduction, minor tip refinement, or straightening a mildly crooked nose.
Best suited for: Dorsal hump reduction, minor tip refinement, narrowing of nasal bones, straightening mild deviations, and patients with thin skin where minimal swelling is advantageous.
Revision Rhinoplasty
Revision rhinoplasty, also called secondary rhinoplasty, addresses unsatisfactory results or complications from previous nasal surgery. This procedure is significantly more complex than primary rhinoplasty due to scar tissue, altered anatomy, and often limited cartilage availability. Revision rates vary, but studies suggest that approximately 10-15% of rhinoplasty patients seek revision surgery.
Common reasons for revision rhinoplasty include persistent breathing difficulties, asymmetry, over-resection leading to a "scooped" or "pinched" appearance, under-correction leaving residual deformities, tip irregularities, and aesthetic dissatisfaction with the overall result. Some revisions address functional issues, while others focus on aesthetic refinement.
The complexity of revision rhinoplasty cannot be overstated. Scar tissue from the previous surgery obscures normal anatomical planes and can make tissue manipulation more difficult. Cartilage that was removed or weakened during the initial surgery may need to be replaced using grafts from the septum, ear, or rib. The altered blood supply and tissue quality can affect healing and final results.
Patients considering revision rhinoplasty should wait at least one year after their primary surgery to allow complete healing and scar maturation. Selecting a surgeon with extensive revision experience is crucial, as this subspecialty requires advanced skills and problem-solving abilities. Many revision rhinoplasty specialists recommend the open approach to allow thorough assessment and reconstruction of the nasal framework.
Best suited for: Correcting unsatisfactory results from previous rhinoplasty, addressing functional problems following surgery, and refining aesthetic outcomes.
Specialized Rhinoplasty Techniques
Preservation Rhinoplasty
Preservation rhinoplasty represents a paradigm shift in surgical philosophy, focusing on maintaining the natural structures of the nose rather than dismantling and reconstructing them. This technique involves lowering the dorsum as a complete unit while preserving the ligamentous attachments and structural integrity of the nose.
Traditional rhinoplasty often involves separating the upper lateral cartilages from the septum, reducing the dorsal height, and then reconstructing the middle vault. Preservation techniques avoid this disruption, potentially leading to more natural-looking results with better long-term stability. The approach has gained significant popularity in recent years, particularly in Europe and among surgeons seeking to achieve subtle, natural-appearing outcomes.
Advantages of preservation rhinoplasty include maintained structural support, potentially reduced swelling and bruising, more natural-looking dorsal lines, and better preservation of the internal nasal valve. However, the technique is not suitable for all cases, particularly those requiring significant dorsal reduction or tip rotation. It works best for patients with relatively straight noses who desire modest dorsal lowering.
Ultrasonic Rhinoplasty
Ultrasonic rhinoplasty utilizes piezoelectric devices that emit ultrasonic vibrations to precisely sculpt nasal bones without damaging surrounding soft tissues. This technology allows surgeons to reshape bone with unprecedented precision while minimizing trauma to adjacent structures such as mucosa, cartilage, and blood vessels.
The piezoelectric device selectively cuts mineralized tissue (bone) while leaving soft tissues intact, reducing bleeding, swelling, and bruising. Surgeons can create smooth, controlled bone cuts and perform delicate maneuvers that would be difficult with traditional instruments. The technique is particularly valuable for dorsal hump reduction, osteotomies (controlled bone fractures to narrow the nose), and cases requiring precise bone sculpting.
Patients who undergo ultrasonic rhinoplasty often experience less post-operative bruising and swelling compared to traditional techniques. The precision of the technology allows for more conservative bone removal and better preservation of structural support. However, the technique requires specialized training and equipment, and not all surgeons offer this option.
The Surgical Process
Understanding what happens during rhinoplasty surgery helps patients feel more prepared and less anxious about the procedure. While specific techniques vary based on individual needs and surgeon preference, the general process follows a predictable sequence.
Pre-Operative Preparation
On the day of surgery, patients arrive at the surgical facility where they complete final paperwork and change into a surgical gown. The surgeon typically meets with the patient to review the surgical plan and answer any last-minute questions. Pre-operative photographs are taken for medical records and comparison purposes. The anesthesiologist discusses anesthesia options and addresses any concerns.
Anesthesia
Rhinoplasty can be performed under general anesthesia or intravenous sedation with local anesthesia, depending on the complexity of the procedure and patient preference. General anesthesia renders the patient completely unconscious, while IV sedation provides deep relaxation with local anesthetic blocking pain. Most surgeons prefer general anesthesia for rhinoplasty as it ensures patient comfort and allows them to focus entirely on the surgical task.
Surgical Steps
Once anesthesia takes effect, the surgeon begins by making the planned incisions—either inside the nostrils for closed rhinoplasty or with an additional columellar incision for open rhinoplasty. The skin and soft tissues are carefully elevated to expose the underlying bone and cartilage framework.
The surgeon then performs the planned modifications, which may include removing a dorsal hump, narrowing the nasal bones through osteotomies, reshaping the tip cartilages, straightening a deviated septum, or placing grafts to provide additional support or contour. Each step requires meticulous attention to detail and constant assessment of how changes affect overall nasal appearance and function.
After completing all modifications, the surgeon carefully repositions the skin and soft tissues over the new nasal framework. Internal incisions are closed with dissolvable sutures. A splint is applied to the outside of the nose to protect the new structure and minimize swelling. Soft internal splints or packing may be placed inside the nostrils to support the septum and control bleeding.
Duration
Rhinoplasty typically takes between 1.5 to 3 hours, depending on the complexity of the case. Revision rhinoplasty or procedures requiring extensive reconstruction may take longer. Surgeons prioritize precision over speed, taking whatever time is necessary to achieve optimal results.